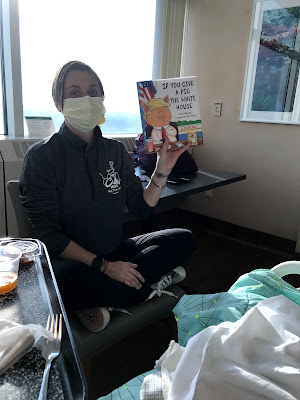
If things proceed as expected, the max chemo is in my body on day 7 of treatment. That was yesterday. Here's a picture of me being disconnected from seven straight days of chemo.
For days 10-14, the maximum killing power of the chemo takes hold and the blood cell counts (and all the other fast-growing cells in my body) are at their lowest. I'm told to expect to need lots of transfusions, lots and lots of rest, and to feel generally really crappy. After a few days, if all goes well, my healthy cells will start their recovery and I'll gradually feel better. What that means, is that I would like visitors, but it is entirely possible that I may change my mind mid-way through the day. Please don't be offended if I either cancel a visit or cut it very short.
Yesterday's counts definitely supported nadir, as have today's:
WBC: 0.2, 0.3 (since the chemo is done, these will slowly start to climb up, but will likely stay pretty low through the next few days before the climb up)
Hemoglobin: 7.4, 7.1
Platelets: 11K, 6K
No blood products needed yesterday, but today I'll get platelets again.
And to kick of the celebration of finishing this first round of chemo, I had the most wonderful morning! Milwaukee does the coolest biking event, called the Santa Rampage. At this event, literally thousands of people dress up as Santa (or elves, etc.) and ride their bikes from Wauwatosa to the lakefront. It's been happening for 15 years, and I'd wanted to ride last year, but caught a cold and it was rainy. I'd determined there was nothing that would stop me from riding in it THIS year. I bought my Santa suit on clearance last year and planned to ride my fat tire bike with all my biking friends. So I was pretty disappointed to not be able to ride in it this year, either.
However, my dear, dear friends, surprised me and found a way for me to participate--they brought the ride to me. :) Barb did the actual ride, and then came to the hospital while Meredith came straight to the hospital and helped me get ready for it. We decorated the exercise bike, Barb wore her Santa stuff, Meredith wore her Christmas sloth outfit, and I had a silly hat. It was amazing (and we made the staff laugh a lot, too).
And then we went back to my room and Meredith cleaned it and decorated it with tinsel and the lights that my friend Chris had brought me.
And because I was so exhausted that I could barely keep my eyes open, Meredith, who is the most awesome K4 teacher ever, read Barb and I a bedtime story. And then I fell fast, fast asleep.
Greg came and watched me sleep, and then I was able to be leave the floor and walk with him to the healing garden--which is amazing. For Milwaukee people, it's like a mini-Domes with giant indoor plants and trees. I will be spending more time there.
And then I was unhooked completely from the IV, took a nice, long shower, and was able to walk without the IV pole for the first time in over a week. I wanted to run, it felt so good.
I was treated to the most spectacular sunset (which my photos cannot do justice to, but up on the 12th floor, you really get to see it from all angles).
Already today there are little annoyances: I feel like I'm getting a cold or something, with a scratchy throat, itchy ears and post-nasal drip; one of my two picc lines appears to be clogged and so they're trying to unclog it, but it hasn't yet responded completely and if not both are working, then I can't get two things (like platelets and IV antibiotics) at the same time. Food still tastes yucky, and I'm just missing my home. But I feel so surrounded by love--both from those who are physically with me, and by all the messages, texts, facebook comments, and just general good feelings. I don't have fear or anxiety--I'm able to just focus on healing. And that is an amazing gift. Thank you all.