And I had a long blog post mostly-completed about this and was waiting till today to post. Unfortunately my computer ate it. So you will get a shorter, less-entertaining post instead.
First of all, this week I spent a LOT of time at Froedtert. I had five days of chemo (M-F), two days of labs and two doctor appointments.
Chemo (Dectabine) is very similar to the first round. That is, three days easy-peasy, followed by feeling tired on day 4 and more icky on day 5 (today). Unfortunately the last three nights I've only gotten somewhere between 4 and 5 hours of sleep. I think, if I remember correctly, that the same thing happened last round. I'll keep better notes for (hopefully) round three. I'm not exhausted--I actually can't sleep because I'm not tired. It's odd. Must be something chemo-related.
Labs have improved ever-so-slightly. Actually, my WBC and neutrophils have creeped down, but they've been essentially zero for a long time anyway. After my last blood transfusion (last Friday), my HGB has maintained, and surprisingly my platelets have increased to 50K! No one seems to know why that's happening, but it's not a bad thing. My peripheral blast counts are bouncing between 5% and 11%.
Monday I had an appointment with Dr. Hamadani and he told me that although he would stay in contact and see me periodically (and manage any GVHD or other transplant-related issues), he was shifting my care back to Dr. Atallah. I also asked about the possibility of a second transplant, and he said that we could only discuss that if (IF) I made it into remission with negative MRD. I think that means that there's not much of a chance that I will end up with negative MRD. But every month may present another option, so I'm not giving up.
Tuesday I met with Dr. Atallah. It was nice to see Dr. Atallah again, even though it meant that I was seeing him because the leukemia is back. He explained more about the clinical trials. Basically, enrollment in clinical trials changes daily, so I can't enroll now anyway. That's because we don't know yet if the Decitabine + Venclexta is working or not. My first chemo cycle was only Decitabine (before the bone marrow biopsy). So the plan is for him to watch my blood blast % and as long as it doesn't get too high, I will be on Venclexta for a full cycle before the next bone marrow biopsy. If that biopsy shows good results, I'll stay on Decitabine + Venclexta until it doesn't work anymore. Then, and only then, we'll look for a clinical trial that might work.
So that's my plan, as it is. Wait and see. And no decisions can really be made until they can be made. :)
I've been trying to stay active, but it's been a lot harder with the heat. I signed up for a few exercise challenges, but one that I was most excited about was the Trek Century Challenge. You could compete at three levels--100, 500 or 1000 miles in the month of July. Last year I rode 322.5 miles in July. I'd planned (last year) to stretch myself and do 500 in 2020. Well, that definitely didn't happen! However I did manage to eke out 100. Given the fact that I had 8 days of chemo and received 7 units of blood and platelets in July, I guess that's really not too bad.
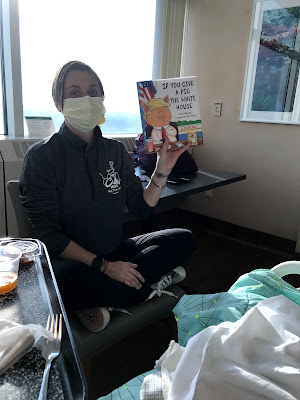
Finally, I have to share the coolest gift that my friend Laura gave me (along with a quick, masked, socially-distant visit):
 |
| a Prince mask--perfect on day +87 (cuz CLASS OF '87 RULES!) |