Just when you think you know the plan, the plan changes.
As I'd written earlier, my breast cancer oncologist referred me to a leukemia specialist in an out of network hospital (Froedtert, for those in the area), not knowing that any other hospital system even offered treatment for leukemia. And lucky for me, through connections, I found excellent providers at Aurora St. Luke's. While there, I also learned that St. Luke's has been doing autologous bone marrow transplants (using your own bone marrow; usually for lymphoma) for years, but that they don't currently do allogenic bone marrow transplants (from a donor; to treat leukemia and myelodysplastic syndromes). However, with two new doctors on staff, who came from institutions where they did allogenic transplants, they are currently training nurses and will start doing allogenics in January.
However, as I began to connect with others in the area who are leukemia survivors, they all received treatment at Froedtert (obviously, as it's the only one in the area). And all raved and raved about Froedtert and pushed me to seek treatment there. And a few encouraged me to reach out to my insurance company to see if there was somewhere I could go where I wouldn't be one of the first patients receiving an allogenic transplant. I knew that my insurance would likely cover UW in Madison, but I just didn't know if it was worth a 90 minute drive for care. After all, being one of the first patients would certainly ensure a lot of observation, right?
Still, on December 19th, I decided to call my insurance company and see about maybe getting a second opinion from UW or another hospital that WAS in network and had more experience with allogenic transplant.
Unlike my first call in November where everyone hemmed and hawed and didn't think they could get me any information for 72 hours or more, this time I was connected with a Cancer Care Specialist familiar with my case, who was adamant that, with my particularly difficult type of leukemia, I needed to be seen at a Center of Excellence (COE) Hospital. They would pay for me to travel to any COE hospital in the country, but the two closest were UW in Madison, and the Mayo Clinic in Rochester. I pushed back and asked why I couldn't go to Froedtert, emphasizing how disruptive it would be for my family if I were treated or hospitalized that far away. The Cancer Care Specialist, in turn, reminded me that it was "only 90 minutes away." She said she would check with her leukemia specialist and get back to me.
Three hours later I got a call back that they learned that Froedtert had better transplant outcomes than either of the COE hospitals they'd suggested. They were recommending that I get my bone marrow transplant at Froedtert, and they actually wanted me to immediately switch care to Froedtert and were looking into how to get Froedtert added to their Center of Excellence hospitals, as they were unsure why they weren't already. EEK!
And then there was a lot of waiting and letting things happen behind the scenes.
Yesterday I had an appointment with Dr. Hamadani who is the director of Froedtert's bone marrow transplant program. He was unaware that my insurance wanted me to transfer all care to Froedtert, so was only prepared to talk about the transplant being done at Froedtert. When I explained that I would be transferring all care, per my insurance, he said he would not be my oncologist (as he doesn't specialize in leukemia), but he would see if Dr. Atallah would see me. (Dr. Atallah, incidentally, is the doctor that all the local Froedtert patients I spoke with saw, and who they credit with saving their lives.)
I also met with the transplant coordinators and learned that Froedtert matches on more proteins/HLAs than St. Luke's does, so if my brother isn't a match, they'll have me re-do the cheek swab for more specific donor matching.
I had blood drawn and learned that Froedtert uses a different kind of picc line that only needs to be flushed weekly, so if care transfers there, I'd either need to learn to flush my own picc line or (their preference) have my current one replaced.
And my labs showed that I needed red blood cells (hemoglobin 7.0), so I was able to get that done at Froedtert instead of having to be driven across town to St. Luke's for the transfusion. So many new processes and procedures. It's interesting to see how a different hospital system does things. And another 8 hour day at a hospital.
Today was a morning of phone calls.
1. I *still* have not received my mail order chemo (Venetoclax), although I should have started on it over a week ago. I am NOT impressed with the specialty pharmacy who didn't call St. Luke's to clarify the dosage (first holdup), or my insurance company to clarify coverage (second holdup), or me to get billing and delivery information (third holdup). After over an hour on the phone answering their annoying questions about how I was feeling about my diagnosis, they finally released the prescription to be delivered "Thursday or maybe Friday." Of course as soon as I learned this, another glitch happened (see below in #4).
2. I heard back from Froedtert's transplant coordinator. Apparently my brother is NOT a match for me. I'm not sure why no one had told us this yet, but now we know. As mentioned above, I'll do another cheek swab to check for more features to match on. The coordinator has utmost confidence that I will get an unrelated donor match. A group of friends is currently working on setting up a Be The Match Event (bone marrow drive) in Milwaukee. When details on that are solidified, I will share them. Out-of-towners will be able to participate by mail, too. (I am moved to tears every time I think about this.)
3. St. Luke's called me to see if I was changing providers or not. This was a really difficult phone call for me, as I have no complaints about my care at St. Luke's and all of the providers (doctors, NPs, nurses, techs, therapists) have been absolutely amazing. I know that I am not "firing" them, but am following my insurance company's preference, and ensuring that I get the best possible outcomes with the most experienced team. Still, it felt cruddy to tell them that I was moving to Froedtert.
4. Froedtert made appointments for me to get my picc line swapped out (Thursday), to set up bi-weekly lab and nurse visits, and to get established with Dr. Atallah. But my initial appointment with Dr. Atallah is scheduled for the day after I am due to start round two of the Vidaza infusions. So I am trying to get that figured out, as I don't want to delay treatment. Froedtert wasn't aware of the start date for my next round, and Dr. Atallah is out today and tomorrow, so hopefully on Thursday that will be worked out. While making these calls, I also learned that Froedtert follows a different procedure to start taking Vinetoclax (including very close watching), and was informed that I should NOT start taking it until Dr. Atallah could review my file and guide me.
5. Froedtert does not routinely schedule visits with cardio-oncology (St. Luke's is well known for its heart care and does things more proactively) so I will keep my appointment for a repeat echocardiogram on Friday at St. Luke's. If that shows no damage, I believe I will only be followed if symptoms appear, but if it does show damage, then I'll need to figure out how to merge two hospital system specialists.
And I think that's it. It's so bizarre to me how there can be so much waiting and not doing a lot, and then BAM! everything happens in a matter of hours.
Tuesday, December 31, 2019
Thursday, December 26, 2019
One round in
Today marks one month since this craziness started. Today was also a crazy long day of appointments at St. Luke's (Greg said it should count as an in-patient day since it was so long), but the best part is that today was day 7 of my first round of the Vidaza chemo. Although I still have frequent appointments (mostly for CBC blood tests), it won't be every single day.
Today started with an appointment in cardio-oncology. Since I have been on three known cardio-toxic meds (Adriamycin, Herceptin, and now Idarubacin), they will follow me closely to see if I look like I'm showing signs of heart failure. I had an echocardiogram done as my baseline before the Idarubacin, and everything looked good at that point (EF 57% and GLS -21, if you are interested in reading what the measurements mean).
So the plan is for me to have a repeat echocardiogram next week.
If there are no changes, then I'll repeat echos in six months and a year, and then annually for five years after treatment (with Idarubacin) is complete.
If there are small changes, then I will continue with echos every six months for a longer time and they will consider cardio-protective medications (ie: blood pressure meds)
If there are big changes, I'll need to do meds and be followed every three months.
The other thing we discussed relates to my QT interval. Three of the meds I'm currently on (fluconazole, the anti-fungal; levofloxacin, the antibiotic; and Zofran, the anti-nausea med) all can interact and impact the QT interval, which can cause an arrhythmia. I will have regular labs drawn to see if my salts are balanced, and I have to watch my symptoms, which are (of course) the same symptoms that are caused by my chemo and/or leukemia/low blood counts. Things like lightheadedness, shortness of breath, racing heart, fatigue.
BUT I did get good news--that I'm encouraged to keep exercising (biking!) and to just listen to my body and rest when it tells me to rest. Greg and I went biking yesterday (so he could try out his new fat tire bike) and a small hill was really, really tough. I had to stop at the top and catch my breath and slow my heart rate. But that's okay--and really due to the fact that my hemoglobin is still very low.
Next stop was labs. My WBCs are still at 0.8 (no neutrophil measures); hemoglobin still hovering around 8 (actually 7.8), and platelets down to 7K.
Then I met with Dr. Sana. He was surprised that I have not yet been able to start the Venetoclax, but it comes from a specialty pharmacy (in Michigan), and they were still working out the dosage earlier this week. Apparently the fluconazole that I have to take is a CYP 3A inhibitor and CYP 3A plays a major role in Venetoclax elimination, so if the two are given together, more Venetoclax is available and the dosage needs to be reduced to avoid over-dosing.
He also clarified a few things going forward.
1. He doesn't plan to do another bone marrow biopsy until 2-3 cycles of the Vidaza are completed.
2. I will be seen 3x/week between the Vidaza infusions for blood work and to determine if I will need blood or platelets.
3. I may not see a rebound in my blood cell counts ("hematological recovery") until three cycles of the chemo is completed.
After that appointment, I got my 7th Vidaza infusion in this first round. This also marks the end (fingers crossed) of needing Zofran, which makes me feel kind of fuzzy, until the next round of Vidaza at least.
And then I got platelets.
It was a long day, and I'm exhausted, but I'm pretty happy to not have to go back in until Monday, I hope!
Today started with an appointment in cardio-oncology. Since I have been on three known cardio-toxic meds (Adriamycin, Herceptin, and now Idarubacin), they will follow me closely to see if I look like I'm showing signs of heart failure. I had an echocardiogram done as my baseline before the Idarubacin, and everything looked good at that point (EF 57% and GLS -21, if you are interested in reading what the measurements mean).
So the plan is for me to have a repeat echocardiogram next week.
If there are no changes, then I'll repeat echos in six months and a year, and then annually for five years after treatment (with Idarubacin) is complete.
If there are small changes, then I will continue with echos every six months for a longer time and they will consider cardio-protective medications (ie: blood pressure meds)
If there are big changes, I'll need to do meds and be followed every three months.
The other thing we discussed relates to my QT interval. Three of the meds I'm currently on (fluconazole, the anti-fungal; levofloxacin, the antibiotic; and Zofran, the anti-nausea med) all can interact and impact the QT interval, which can cause an arrhythmia. I will have regular labs drawn to see if my salts are balanced, and I have to watch my symptoms, which are (of course) the same symptoms that are caused by my chemo and/or leukemia/low blood counts. Things like lightheadedness, shortness of breath, racing heart, fatigue.
BUT I did get good news--that I'm encouraged to keep exercising (biking!) and to just listen to my body and rest when it tells me to rest. Greg and I went biking yesterday (so he could try out his new fat tire bike) and a small hill was really, really tough. I had to stop at the top and catch my breath and slow my heart rate. But that's okay--and really due to the fact that my hemoglobin is still very low.
Next stop was labs. My WBCs are still at 0.8 (no neutrophil measures); hemoglobin still hovering around 8 (actually 7.8), and platelets down to 7K.
Then I met with Dr. Sana. He was surprised that I have not yet been able to start the Venetoclax, but it comes from a specialty pharmacy (in Michigan), and they were still working out the dosage earlier this week. Apparently the fluconazole that I have to take is a CYP 3A inhibitor and CYP 3A plays a major role in Venetoclax elimination, so if the two are given together, more Venetoclax is available and the dosage needs to be reduced to avoid over-dosing.
He also clarified a few things going forward.
1. He doesn't plan to do another bone marrow biopsy until 2-3 cycles of the Vidaza are completed.
2. I will be seen 3x/week between the Vidaza infusions for blood work and to determine if I will need blood or platelets.
3. I may not see a rebound in my blood cell counts ("hematological recovery") until three cycles of the chemo is completed.
After that appointment, I got my 7th Vidaza infusion in this first round. This also marks the end (fingers crossed) of needing Zofran, which makes me feel kind of fuzzy, until the next round of Vidaza at least.
And then I got platelets.
It was a long day, and I'm exhausted, but I'm pretty happy to not have to go back in until Monday, I hope!
Monday, December 23, 2019
Home Sweet Home
I realized that not everyone is on Facebook and so not everyone knew that I had, in fact, made it home. Friday, after my second infusion of the Vidaza (chemo), I was released from the hospital. I have a long list of potential things that can happen (fever, allergic stuff, etc.) and a huge bunch of meds to take, but I'm home!
The Vidaza is administered IV infusion for seven days in a row, and then 21 days off. After the first two in the hospital, I got my second two at the Vince Lombardi Cancer Center (also in the hospital, but as an outpatient), and today was #5 in the infusion center in Medical Office Building 3 on the 9th floor. I'll have #6 tomorrow, take Xmas day off, and then #7 on the 26th.
I also learned that my insurance approved me to take the oral chemo Venetoclax (one big hurdle), and it will be shipped by specialty pharmacy or something. But (of course) there was an issue because I should be taking allopurinol (to protect my kidneys from tumor lysis syndrome) but the allopurinol caused the nasty red rash on my stomach, and apparently a skin rash is the first sign that it could be anaphylactic, so no more allopurinol for me. The alternative med (uloric) has been associated with an increase in heart issues, and I'm on so many cardiotoxic meds already that they've decided it is safer to monitor my levels of uric acid and NOT give me uloric unless it's needed.
The other thing we're waiting on is what dose level of Venetoclax I will receive. Apparently it interacts with Fluconazole (the anti-fungal I need since I have essentially no immune system), and so I may need to do a dose-reduction. Hopefully that will all be figured out and the meds will be ordered, and I can start on that soon. I was happy to hear that Venetoclax carries a "low risk of nausea" and so I am hopeful that I can get by without taking Zofran (which I get before the Vidaza). It's a crazy string of meds that lead to other meds and all sorts of delightful side effects.
But I have been adjusting pretty well to being out of the hospital after 21 days (22 if you count the first night I was admitted). It was very odd when I first got home. Though it was nice to be home, it didn't really feel like "home" because I'd been in the hospital for so long. I'm happy to say that I was able to get over that relatively quickly. It's the little things--like the first night I was home, I minced an onion for a recipe. On Sunday I actually drove to chemo (Cara drove me home because the anti-nausea meds make me kind of sleepy and dizzy). I have been walking, and yesterday I even went for a five mile bike ride on my fat tire bike!
Cara & Travis are home for the break between semesters, and Ash is also off. It's been wonderful and cozy to be home playing games and cooking and being kind of lazy, actually.
And my white blood cells are creeping up very, very slowly. Yesterday they were able to measure my neutrophils (0.1) but today, although my total WBCs were higher, they didn't check the neutrophils. Maybe tomorrow...
I wish everyone a wonderful holiday--whatever you celebrate(d). The days are getting longer now--which will take forever to seem like a difference, but mentally it's nice to know. And 50 degrees in December? I certainly can't complain--especially when it includes lots of sunshine. So many things to be thankful for.
The Vidaza is administered IV infusion for seven days in a row, and then 21 days off. After the first two in the hospital, I got my second two at the Vince Lombardi Cancer Center (also in the hospital, but as an outpatient), and today was #5 in the infusion center in Medical Office Building 3 on the 9th floor. I'll have #6 tomorrow, take Xmas day off, and then #7 on the 26th.
I also learned that my insurance approved me to take the oral chemo Venetoclax (one big hurdle), and it will be shipped by specialty pharmacy or something. But (of course) there was an issue because I should be taking allopurinol (to protect my kidneys from tumor lysis syndrome) but the allopurinol caused the nasty red rash on my stomach, and apparently a skin rash is the first sign that it could be anaphylactic, so no more allopurinol for me. The alternative med (uloric) has been associated with an increase in heart issues, and I'm on so many cardiotoxic meds already that they've decided it is safer to monitor my levels of uric acid and NOT give me uloric unless it's needed.
The other thing we're waiting on is what dose level of Venetoclax I will receive. Apparently it interacts with Fluconazole (the anti-fungal I need since I have essentially no immune system), and so I may need to do a dose-reduction. Hopefully that will all be figured out and the meds will be ordered, and I can start on that soon. I was happy to hear that Venetoclax carries a "low risk of nausea" and so I am hopeful that I can get by without taking Zofran (which I get before the Vidaza). It's a crazy string of meds that lead to other meds and all sorts of delightful side effects.
But I have been adjusting pretty well to being out of the hospital after 21 days (22 if you count the first night I was admitted). It was very odd when I first got home. Though it was nice to be home, it didn't really feel like "home" because I'd been in the hospital for so long. I'm happy to say that I was able to get over that relatively quickly. It's the little things--like the first night I was home, I minced an onion for a recipe. On Sunday I actually drove to chemo (Cara drove me home because the anti-nausea meds make me kind of sleepy and dizzy). I have been walking, and yesterday I even went for a five mile bike ride on my fat tire bike!
Cara & Travis are home for the break between semesters, and Ash is also off. It's been wonderful and cozy to be home playing games and cooking and being kind of lazy, actually.
And my white blood cells are creeping up very, very slowly. Yesterday they were able to measure my neutrophils (0.1) but today, although my total WBCs were higher, they didn't check the neutrophils. Maybe tomorrow...
I wish everyone a wonderful holiday--whatever you celebrate(d). The days are getting longer now--which will take forever to seem like a difference, but mentally it's nice to know. And 50 degrees in December? I certainly can't complain--especially when it includes lots of sunshine. So many things to be thankful for.
Thursday, December 19, 2019
Another stop on the bullet train
Last time I blogged, the plan was to get my neutrophils up (usually happens on about day 21; today is day 20) so I can be hit with the next regimen of chemo. (Thank you for positive neutrophil vibes--unfortunately they're still not back.)
Yesterday on rounds, the doctor said that sometimes with leukemia the red blood cells and platelets will rebound (mine are doing that, slowly and surely), but the white blood cells may not. This is particularly true when you initially present with a low white blood cell count and not a high one. (Also me.) And that if my neutrophils didn't rebound by this weekend, they would start on the new regimen while I was still in-patient, which would allow me to be watched closely for reactions and adverse effects for the first two days of treatment. They would then, if I was stable, allow me to go home in time for Christmas (!!!!!).
This morning on rounds, the doctor and NPs came in and the first thing they said was, "want to get started on Vidaza today?" I gave a resounding "yes" as the sooner I start, the sooner I'm fighting the leukemic bone marrow and the sooner I'm done with round one and (hopefully) the sooner I can go home. Dr. Sana said if I did okay today and tomorrow I could potentially be released tomorrow (Friday) night.
I know that things can still happen--I may react poorly to the chemo, spike a fever, have other things pop up... But the idea that I might be home tomorrow--TOMORROW--has made today a phenomenal day. And I've been quite bossy, saddling my family with a list of cleaning and shopping chores to prepare for me coming home.
My fingers are so tightly crossed that this goes as planned and I need only sleep one more night in this hospital bed. I'm almost afraid to say it out loud.
p.s. I haven't needed blood since December 11th or platelets since December 15th. I hope I keep holding my own, although I'm sure the new chemo will knock me down again. If I kept track of your postings on social media, I'm pretty close to having replenished what I used. At least of the blood--platelets are much harder. Thank you, thank you, thank you!
Yesterday on rounds, the doctor said that sometimes with leukemia the red blood cells and platelets will rebound (mine are doing that, slowly and surely), but the white blood cells may not. This is particularly true when you initially present with a low white blood cell count and not a high one. (Also me.) And that if my neutrophils didn't rebound by this weekend, they would start on the new regimen while I was still in-patient, which would allow me to be watched closely for reactions and adverse effects for the first two days of treatment. They would then, if I was stable, allow me to go home in time for Christmas (!!!!!).
This morning on rounds, the doctor and NPs came in and the first thing they said was, "want to get started on Vidaza today?" I gave a resounding "yes" as the sooner I start, the sooner I'm fighting the leukemic bone marrow and the sooner I'm done with round one and (hopefully) the sooner I can go home. Dr. Sana said if I did okay today and tomorrow I could potentially be released tomorrow (Friday) night.
I know that things can still happen--I may react poorly to the chemo, spike a fever, have other things pop up... But the idea that I might be home tomorrow--TOMORROW--has made today a phenomenal day. And I've been quite bossy, saddling my family with a list of cleaning and shopping chores to prepare for me coming home.
My fingers are so tightly crossed that this goes as planned and I need only sleep one more night in this hospital bed. I'm almost afraid to say it out loud.
p.s. I haven't needed blood since December 11th or platelets since December 15th. I hope I keep holding my own, although I'm sure the new chemo will knock me down again. If I kept track of your postings on social media, I'm pretty close to having replenished what I used. At least of the blood--platelets are much harder. Thank you, thank you, thank you!
Wednesday, December 18, 2019
Not the results I'd hoped for.
After days (that seemed like weeks) of waiting, the results of my bone marrow biopsy and the final genetic testing results (next gen sequencing) of my leukemia both came in on Tuesday afternoon.
The first hope, that the bone marrow would be hypoplastic ("empty") and that the blasts would be under 5%, was not met. I have between 15-20% blasts still in my marrow. I had started with 40%.
This was not completely unexpected, as some of the genetic information came out over the last few days. If what was suspected was true, the 7+3 chemo was not a good match for my particular leukemia. While this is frustrating, I was in a bad enough condition upon admission that *something* had to be done, and so it wasn't a terrible idea to start with the 7+3. (Apparently some cancer hospitals do hold off on any treatment until they get the results from the genetic testing.)
Leukemia is not staged like other cancers. Instead, one of the ways it's grouped is by the favorability of the outcome. Best is "favorable;" worst is "unfavorable" or "adverse;" and in between is intermediate. These are the best guesses as to whether the leukemia will respond to chemo and go into remission. And remission must be obtained before a bone marrow transplant is attempted. (If you leave leukemic bone marrow and put new bone marrow in, they'll compete and the leukemic bone marrow will eventually win.)
My leukemia, unfortunately, has a lot of unfavorable things going for it.
1. Being treatment-associated AML (t-AML) automatically makes it less favorable
2. Having greater than three chromosomal mutations is unfavorable; my leukemia has fourteen(!)
3. One particular gene deletion is highly unfavorable--p53 (involved in signaling for such important things as cell cycle arrest, apoptosis/cell death, and DNA repair). And I have only one copy of p53.
But we have a plan to move forward, and it takes into account the p53 aspect.
There are two chemotherapies that are recently out of Stage 2 Clinical Trial (I think... maybe only one, or the combo?), as tested on elderly patients. If you're into that kind of thing, I think this is the paper my doctor referred to. Although I did not achieve complete remission with the first chemo regimen, this is not a second attempt (ie: failure of first attempt) but a re-induction--or a second first attempt.
I will receive a 7 day infusion of Vidaza (azacitidine), separated by 21 "rest" days and will get that 2-3 times. I will also take a daily oral chemo called Venclexta (venetoclax). The hope is that this regimen will put me into remission. The best part in my mind right now is that they are both done as outpatient treatments.
(For those who are fascinated with the genetic components, Vidaza is a hypermethylating agent--which would turn on the defective p53 and Venetoclax blocks the BCL2 protein, which would allow apoptosis.)
Before I can go home, and before I am considered recovered enough from the first round of chemo, I need to get my neutrophils up to 0.5. They're currently too low to measure, although my total white blood cell count is slowly increasing, and neutrophils are a subset of white blood cells, so I'm hoping that they, too, will soon start to inch up.
Time to switch that positive energy into making my neutrophils rebound so I can get home and so I can start on the new chemo.
It's a plan and I always do much better with a plan.
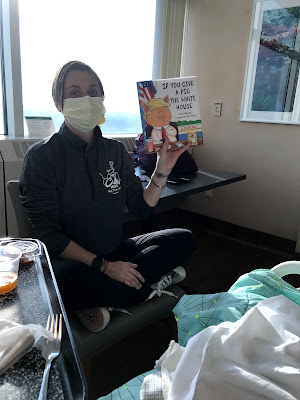
And I need to get home to this:
The first hope, that the bone marrow would be hypoplastic ("empty") and that the blasts would be under 5%, was not met. I have between 15-20% blasts still in my marrow. I had started with 40%.
This was not completely unexpected, as some of the genetic information came out over the last few days. If what was suspected was true, the 7+3 chemo was not a good match for my particular leukemia. While this is frustrating, I was in a bad enough condition upon admission that *something* had to be done, and so it wasn't a terrible idea to start with the 7+3. (Apparently some cancer hospitals do hold off on any treatment until they get the results from the genetic testing.)
Leukemia is not staged like other cancers. Instead, one of the ways it's grouped is by the favorability of the outcome. Best is "favorable;" worst is "unfavorable" or "adverse;" and in between is intermediate. These are the best guesses as to whether the leukemia will respond to chemo and go into remission. And remission must be obtained before a bone marrow transplant is attempted. (If you leave leukemic bone marrow and put new bone marrow in, they'll compete and the leukemic bone marrow will eventually win.)
My leukemia, unfortunately, has a lot of unfavorable things going for it.
1. Being treatment-associated AML (t-AML) automatically makes it less favorable
2. Having greater than three chromosomal mutations is unfavorable; my leukemia has fourteen(!)
3. One particular gene deletion is highly unfavorable--p53 (involved in signaling for such important things as cell cycle arrest, apoptosis/cell death, and DNA repair). And I have only one copy of p53.
But we have a plan to move forward, and it takes into account the p53 aspect.
There are two chemotherapies that are recently out of Stage 2 Clinical Trial (I think... maybe only one, or the combo?), as tested on elderly patients. If you're into that kind of thing, I think this is the paper my doctor referred to. Although I did not achieve complete remission with the first chemo regimen, this is not a second attempt (ie: failure of first attempt) but a re-induction--or a second first attempt.
I will receive a 7 day infusion of Vidaza (azacitidine), separated by 21 "rest" days and will get that 2-3 times. I will also take a daily oral chemo called Venclexta (venetoclax). The hope is that this regimen will put me into remission. The best part in my mind right now is that they are both done as outpatient treatments.
(For those who are fascinated with the genetic components, Vidaza is a hypermethylating agent--which would turn on the defective p53 and Venetoclax blocks the BCL2 protein, which would allow apoptosis.)
Before I can go home, and before I am considered recovered enough from the first round of chemo, I need to get my neutrophils up to 0.5. They're currently too low to measure, although my total white blood cell count is slowly increasing, and neutrophils are a subset of white blood cells, so I'm hoping that they, too, will soon start to inch up.
Time to switch that positive energy into making my neutrophils rebound so I can get home and so I can start on the new chemo.
It's a plan and I always do much better with a plan.
And I need to get home to this:
Wednesday, December 11, 2019
The plan, clarified
Monday I finally got to meet the new chair of the St. Luke's Hematological Oncology group: Dr. Medlin. I have heard so much good about him from all the staff. And he's great. Down-to-earth, answers questions at the level I've asked (he asked my background to clarify), positive, confident.
We spent time talking about the plan for my treatment, which didn't change from what others had told me, but which was clarified somewhat.
We started with induction chemo to get my body to go into remission. We will know if that was achieved (or at least the first step toward achieving it) when we get the results from Friday's bone marrow biopsy. So yes, the bone marrow biopsy will be done on Friday. Results will take a "few days." There are two goals:
If either of these things are not achieved, then stage one was not effective and we need to do another, different round of induction chemo. This is the stage that makes my heart race. This would prevent me from being home for Christmas, and it would certainly be a "harder" chemo on my body, plus just an addition chemo in general. But Dr. Medlin did a great job of explaining why this is an important step and why, if this happens, it is not the worst possible thing. Previously, treatment involved this 7+3 chemo, then the rounds that follow (I'll get into that shortly), but they were not able to determine if the chemo was actually effective. So you'd go through the whole process and not even have received remission, which meant that it was not going to be effective. Adding this step, and the sensitivity that is now achievable, means that more people are in true remission and have better outcomes. I like better outcomes.
Next step, once that first round of remission is achieved, is to do four rounds of maintenance/consolidation. Dr. Medlin explained that, even when there may be no evidence of cancer cells, there are still likely as many as 10^12 cells in the body (the "undetectable level"). Much like how many breast or other solid tumor cancer patients may have surgery with clean margins and clean nodes, but still have chemo after, that is the purpose of the chemo.
And then we move on to the bone marrow transplant. There are only three options for an allogenic donor:
We spent time talking about the plan for my treatment, which didn't change from what others had told me, but which was clarified somewhat.
We started with induction chemo to get my body to go into remission. We will know if that was achieved (or at least the first step toward achieving it) when we get the results from Friday's bone marrow biopsy. So yes, the bone marrow biopsy will be done on Friday. Results will take a "few days." There are two goals:
- The bone marrow is essentially empty. We want less than 5% of cells within the bone marrow, which indicates that the chemo cleaned it all out.
- Of the cells left in the bone marrow, less than 5% of them are blasts (cancerous cells).
If either of these things are not achieved, then stage one was not effective and we need to do another, different round of induction chemo. This is the stage that makes my heart race. This would prevent me from being home for Christmas, and it would certainly be a "harder" chemo on my body, plus just an addition chemo in general. But Dr. Medlin did a great job of explaining why this is an important step and why, if this happens, it is not the worst possible thing. Previously, treatment involved this 7+3 chemo, then the rounds that follow (I'll get into that shortly), but they were not able to determine if the chemo was actually effective. So you'd go through the whole process and not even have received remission, which meant that it was not going to be effective. Adding this step, and the sensitivity that is now achievable, means that more people are in true remission and have better outcomes. I like better outcomes.
Next step, once that first round of remission is achieved, is to do four rounds of maintenance/consolidation. Dr. Medlin explained that, even when there may be no evidence of cancer cells, there are still likely as many as 10^12 cells in the body (the "undetectable level"). Much like how many breast or other solid tumor cancer patients may have surgery with clean margins and clean nodes, but still have chemo after, that is the purpose of the chemo.
And then we move on to the bone marrow transplant. There are only three options for an allogenic donor:
- A full-match sibling, matching on 6 of 6 Human Leucocyte Antigens (HLAs)
- An unrelated perfect donor, matching on 10 of 10 HLAs
- A haplo-identical donor, like a child, matching on 5 of 10 HLAs
The reason you can use a half match with only 5 of 10 is that you'd only use a related haplo donor, and there are many other factors that aren't tested/matched on, but are also important and helpful in minimizing the likelihood and severity of graft vs. host disease (GVHD). These factors tend to clump together in familial lines, so while the third option is riskier, it can be done.
I'm trying not to think about the fact that finding a donor is an "if" and not necessarily a "when." There are certainly many people who do not find a donor by any of those three means. But I'm also hoping that karma, and all my wonderful loved ones who have recently signed up to "Be The Match" have someone or else on the other side of the world with just as many amazing loved ones signing up for them and somehow we'll all end up matched.
As far as preparation for a bone marrow transplant, it is another chemo regimen of 5-7 days. Full body radiation is not usually used in AML (more often in ALL), so probably not necessary. And then the transplant itself is relatively simple--just like a blood transfusion. The hardest/worst part is waiting to see if it takes and how bad the GVHD is. I have decided not to look too far into that at this point.
---------
Other than that, I'm just keeping on here in Nadir-land. Still having the lovely GI issues. My new antibiotic (meropenen, since I developed that rash in response to the cephapine) seems to give me a headache. At least, both times I've received it, I've developed a headache at the base of my skull within a few minutes of the IV beginning. Last night I slept through most of it, but this morning it is still with me. Even a visit from massage therapy and some essential oils only slightly tamed it.
With the new blood thresholds, I needed both blood and platelets last night, which made for a long night with all the vitals checks that they do before, during and after receiving blood product. This morning my counts were sufficient enough that I didn't need any product (WBC: 0.3; HGB: 8.3; PLT: 71K). Next draw is at 10:00 am and I'm crossing fingers that I'm holding onto things well enough to not need more. I don't know how long I'll be at these higher thresholds. Hopefully my own cells will start coming back soon and that will both decrease the need for the transfusions and prepare me for possible release from the hospital.
Whether it's the interruptions last night, or day 12 post-chemo (3 of 5 Nadir), I'm thinking I might actually need a morning nap today. I'm pretty happy that it's another beautifully sunny day. I hear it's cold outside, but I wouldn't know that from my room. :)
Tuesday, December 10, 2019
Lower counts and little issues
When I blogged about Nadir last, I mistakenly stated/remembered that it was days 7-10 after starting chemo. So I was pretty happy that I did pretty well this weekend, just needing a little more rest, and was looking forward to Monday (Day 10) being over the worst and moving on. And then my nurse said something like, "just remember that days 10-14 can be very intense and some people lose their appetite and really do need to take those naps that you are trying to avoid, and it can be a rough couple of days." And then I remembered that Nadir is 10-14, and not 7-10. I wasn't just getting out of it, it was just getting INTO it.
My counts continue to remain low:
WBCs holding steady at 0.3 the last few tests
HGB bouncing around 6.4, 7.7, 6.7, 7.3
Platelets also bouncing 14K, 33K, 20K, 43K
I received both blood and platelets yesterday even through my platelet level was above the cut-off. I'll get more of both today, too. (More on that later.)
--------
My wonderful, generous friend, Team Phoenix sister, and leukemia survivor Vanessa came to visit yesterday. Vanessa immediately reached out to me when she heard of my diagnosis and has provided such a "been there" perspective since the start. Talking with her yesterday in person was wonderful. She also works for an organization called Tricia's Troops, which provides all sorts of amazing support to all kinds of cancer patients all over Southeastern Wisconsin. Vanessa brought me a lovely chemo support bag, and the group helps with things like housework or child care or transportation. If you're a cancer patient (or love one), check them out. And if you're looking for a place to donate, also check them out.
And after a not-terribly-long visit with Vanessa, I absolutely crashed and slept all afternoon. Guess this exhaustion thing is no joke. I had a few hours of awake time, visited with Greg and Ash, and was asleep again before 9:00 pm. Wow.
Unfortunately, what's been overlaying all of this for the last two days is a troubling side effect of, I assume, the chemo. I was showing some signs of a possible GI tract bleed, which resulted in lots of (not) fun observations and measurements. While I haven't been nauseous (knock wood), my stomach has been ouchie (for lack of a technical term), and I've developed heartburn, and some intestinal cramping. Just enough for my comment of, "I'm in no pain," to no longer hold 100%. So it's caused some changes in protocol. They bumped up my blood count tests from 24 hours to 12 hours (and now 6 hours). They immediately gave me more platelets, regardless of my count, and they changed the cutoff from 10K to 25K (it has since risen to 50K). I also got whole blood and the HGB cut-off is raised from 7.0 to 8.0. From what I can tell (supported by research that my amazing PH researcher friend Susan has done), this GI stuff is very common with these chemo meds (the bleeding less so, but we're working on that). And I'm on two antibiotics, which always impact my stomach. The most frustrating thing is that when the stomach cramping hits, it hits. So I've been afraid to walk as much and be far from my room, and going down to the Healing Garden seems way too far. These both make me sad. I'm hoping that the bleeding stops soon so I won't be burning through the platelets so quickly.
-----
Finishing this blog with stuff about today.
Day 11 was pretty similar to day 10. I had a pretty productive morning with several cool visits, and then a complete crash shortly after noon. After a nice snooze in the sun, and a visit from massage therapy, and a shower and a walk around the floor and in the healing garden (without an IV!), I'm back in my room, hooked up to fluids, awaiting the latest CBC counts to see if I need more platelets, and I also just found out that they think the rash on my stomach is in response to one of the IV antibiotics that I'm on (Cefapine). So I'll be switching from that one tonight. Unfortunately, instead of a half hour run time, the new one will be an hour and a half, but only once a day. I hate to be running out of antibiotics I can use, as I'll be on a lot of antibiotics for a long time.
And I had a little more energy today than yesterday. I'm not back to walking as much (and haven't been on the exercise bike), but I was able to add the squats back into my walk this afternoon. I was thrilled to see another patient working hard on strength exercises at one of the windows as I made my circuit.
I did get to meet the (new) Chair of the department yesterday and had a long talk with him about my plan. I'll try to write that up tomorrow. Until then, keep visualizing my bone marrow being completely destroyed and cheer with me when I feel crappy, because that's probably a sign that it's working. :) 2/5 days of Nadir in. I can do this!
My counts continue to remain low:
WBCs holding steady at 0.3 the last few tests
HGB bouncing around 6.4, 7.7, 6.7, 7.3
Platelets also bouncing 14K, 33K, 20K, 43K
I received both blood and platelets yesterday even through my platelet level was above the cut-off. I'll get more of both today, too. (More on that later.)
--------
My wonderful, generous friend, Team Phoenix sister, and leukemia survivor Vanessa came to visit yesterday. Vanessa immediately reached out to me when she heard of my diagnosis and has provided such a "been there" perspective since the start. Talking with her yesterday in person was wonderful. She also works for an organization called Tricia's Troops, which provides all sorts of amazing support to all kinds of cancer patients all over Southeastern Wisconsin. Vanessa brought me a lovely chemo support bag, and the group helps with things like housework or child care or transportation. If you're a cancer patient (or love one), check them out. And if you're looking for a place to donate, also check them out.
And after a not-terribly-long visit with Vanessa, I absolutely crashed and slept all afternoon. Guess this exhaustion thing is no joke. I had a few hours of awake time, visited with Greg and Ash, and was asleep again before 9:00 pm. Wow.
Unfortunately, what's been overlaying all of this for the last two days is a troubling side effect of, I assume, the chemo. I was showing some signs of a possible GI tract bleed, which resulted in lots of (not) fun observations and measurements. While I haven't been nauseous (knock wood), my stomach has been ouchie (for lack of a technical term), and I've developed heartburn, and some intestinal cramping. Just enough for my comment of, "I'm in no pain," to no longer hold 100%. So it's caused some changes in protocol. They bumped up my blood count tests from 24 hours to 12 hours (and now 6 hours). They immediately gave me more platelets, regardless of my count, and they changed the cutoff from 10K to 25K (it has since risen to 50K). I also got whole blood and the HGB cut-off is raised from 7.0 to 8.0. From what I can tell (supported by research that my amazing PH researcher friend Susan has done), this GI stuff is very common with these chemo meds (the bleeding less so, but we're working on that). And I'm on two antibiotics, which always impact my stomach. The most frustrating thing is that when the stomach cramping hits, it hits. So I've been afraid to walk as much and be far from my room, and going down to the Healing Garden seems way too far. These both make me sad. I'm hoping that the bleeding stops soon so I won't be burning through the platelets so quickly.
-----
Finishing this blog with stuff about today.
Day 11 was pretty similar to day 10. I had a pretty productive morning with several cool visits, and then a complete crash shortly after noon. After a nice snooze in the sun, and a visit from massage therapy, and a shower and a walk around the floor and in the healing garden (without an IV!), I'm back in my room, hooked up to fluids, awaiting the latest CBC counts to see if I need more platelets, and I also just found out that they think the rash on my stomach is in response to one of the IV antibiotics that I'm on (Cefapine). So I'll be switching from that one tonight. Unfortunately, instead of a half hour run time, the new one will be an hour and a half, but only once a day. I hate to be running out of antibiotics I can use, as I'll be on a lot of antibiotics for a long time.
And I had a little more energy today than yesterday. I'm not back to walking as much (and haven't been on the exercise bike), but I was able to add the squats back into my walk this afternoon. I was thrilled to see another patient working hard on strength exercises at one of the windows as I made my circuit.
I did get to meet the (new) Chair of the department yesterday and had a long talk with him about my plan. I'll try to write that up tomorrow. Until then, keep visualizing my bone marrow being completely destroyed and cheer with me when I feel crappy, because that's probably a sign that it's working. :) 2/5 days of Nadir in. I can do this!
Sunday, December 8, 2019
Now entering Nadir
I've written about nadir before--essentially the low point in blood counts after chemo is given. But nadir after leukemia chemo is even more intense than it was during breast cancer treatment.
If things proceed as expected, the max chemo is in my body on day 7 of treatment. That was yesterday. Here's a picture of me being disconnected from seven straight days of chemo.
For days 10-14, the maximum killing power of the chemo takes hold and the blood cell counts (and all the other fast-growing cells in my body) are at their lowest. I'm told to expect to need lots of transfusions, lots and lots of rest, and to feel generally really crappy. After a few days, if all goes well, my healthy cells will start their recovery and I'll gradually feel better. What that means, is that I would like visitors, but it is entirely possible that I may change my mind mid-way through the day. Please don't be offended if I either cancel a visit or cut it very short.
Yesterday's counts definitely supported nadir, as have today's:
WBC: 0.2, 0.3 (since the chemo is done, these will slowly start to climb up, but will likely stay pretty low through the next few days before the climb up)
Hemoglobin: 7.4, 7.1
Platelets: 11K, 6K
No blood products needed yesterday, but today I'll get platelets again.
And to kick of the celebration of finishing this first round of chemo, I had the most wonderful morning! Milwaukee does the coolest biking event, called the Santa Rampage. At this event, literally thousands of people dress up as Santa (or elves, etc.) and ride their bikes from Wauwatosa to the lakefront. It's been happening for 15 years, and I'd wanted to ride last year, but caught a cold and it was rainy. I'd determined there was nothing that would stop me from riding in it THIS year. I bought my Santa suit on clearance last year and planned to ride my fat tire bike with all my biking friends. So I was pretty disappointed to not be able to ride in it this year, either.
However, my dear, dear friends, surprised me and found a way for me to participate--they brought the ride to me. :) Barb did the actual ride, and then came to the hospital while Meredith came straight to the hospital and helped me get ready for it. We decorated the exercise bike, Barb wore her Santa stuff, Meredith wore her Christmas sloth outfit, and I had a silly hat. It was amazing (and we made the staff laugh a lot, too).
And then we went back to my room and Meredith cleaned it and decorated it with tinsel and the lights that my friend Chris had brought me.
And because I was so exhausted that I could barely keep my eyes open, Meredith, who is the most awesome K4 teacher ever, read Barb and I a bedtime story. And then I fell fast, fast asleep.
Greg came and watched me sleep, and then I was able to be leave the floor and walk with him to the healing garden--which is amazing. For Milwaukee people, it's like a mini-Domes with giant indoor plants and trees. I will be spending more time there.
And then I was unhooked completely from the IV, took a nice, long shower, and was able to walk without the IV pole for the first time in over a week. I wanted to run, it felt so good.
I was treated to the most spectacular sunset (which my photos cannot do justice to, but up on the 12th floor, you really get to see it from all angles).
And I had a long, barely-interrupted night of sleep.
Already today there are little annoyances: I feel like I'm getting a cold or something, with a scratchy throat, itchy ears and post-nasal drip; one of my two picc lines appears to be clogged and so they're trying to unclog it, but it hasn't yet responded completely and if not both are working, then I can't get two things (like platelets and IV antibiotics) at the same time. Food still tastes yucky, and I'm just missing my home. But I feel so surrounded by love--both from those who are physically with me, and by all the messages, texts, facebook comments, and just general good feelings. I don't have fear or anxiety--I'm able to just focus on healing. And that is an amazing gift. Thank you all.
If things proceed as expected, the max chemo is in my body on day 7 of treatment. That was yesterday. Here's a picture of me being disconnected from seven straight days of chemo.
For days 10-14, the maximum killing power of the chemo takes hold and the blood cell counts (and all the other fast-growing cells in my body) are at their lowest. I'm told to expect to need lots of transfusions, lots and lots of rest, and to feel generally really crappy. After a few days, if all goes well, my healthy cells will start their recovery and I'll gradually feel better. What that means, is that I would like visitors, but it is entirely possible that I may change my mind mid-way through the day. Please don't be offended if I either cancel a visit or cut it very short.
Yesterday's counts definitely supported nadir, as have today's:
WBC: 0.2, 0.3 (since the chemo is done, these will slowly start to climb up, but will likely stay pretty low through the next few days before the climb up)
Hemoglobin: 7.4, 7.1
Platelets: 11K, 6K
No blood products needed yesterday, but today I'll get platelets again.
And to kick of the celebration of finishing this first round of chemo, I had the most wonderful morning! Milwaukee does the coolest biking event, called the Santa Rampage. At this event, literally thousands of people dress up as Santa (or elves, etc.) and ride their bikes from Wauwatosa to the lakefront. It's been happening for 15 years, and I'd wanted to ride last year, but caught a cold and it was rainy. I'd determined there was nothing that would stop me from riding in it THIS year. I bought my Santa suit on clearance last year and planned to ride my fat tire bike with all my biking friends. So I was pretty disappointed to not be able to ride in it this year, either.
However, my dear, dear friends, surprised me and found a way for me to participate--they brought the ride to me. :) Barb did the actual ride, and then came to the hospital while Meredith came straight to the hospital and helped me get ready for it. We decorated the exercise bike, Barb wore her Santa stuff, Meredith wore her Christmas sloth outfit, and I had a silly hat. It was amazing (and we made the staff laugh a lot, too).
And then we went back to my room and Meredith cleaned it and decorated it with tinsel and the lights that my friend Chris had brought me.
And because I was so exhausted that I could barely keep my eyes open, Meredith, who is the most awesome K4 teacher ever, read Barb and I a bedtime story. And then I fell fast, fast asleep.
Greg came and watched me sleep, and then I was able to be leave the floor and walk with him to the healing garden--which is amazing. For Milwaukee people, it's like a mini-Domes with giant indoor plants and trees. I will be spending more time there.
And then I was unhooked completely from the IV, took a nice, long shower, and was able to walk without the IV pole for the first time in over a week. I wanted to run, it felt so good.
I was treated to the most spectacular sunset (which my photos cannot do justice to, but up on the 12th floor, you really get to see it from all angles).
Already today there are little annoyances: I feel like I'm getting a cold or something, with a scratchy throat, itchy ears and post-nasal drip; one of my two picc lines appears to be clogged and so they're trying to unclog it, but it hasn't yet responded completely and if not both are working, then I can't get two things (like platelets and IV antibiotics) at the same time. Food still tastes yucky, and I'm just missing my home. But I feel so surrounded by love--both from those who are physically with me, and by all the messages, texts, facebook comments, and just general good feelings. I don't have fear or anxiety--I'm able to just focus on healing. And that is an amazing gift. Thank you all.
Friday, December 6, 2019
Nearing the end of the first big step
Today's a big day. This morning they hung the final bag of my 7+3 chemo regimen. Unfortunately, each bag is a little more than 24 hours, so I won't be done till sometime tomorrow afternoon, but there is an end in sight!
Counts still dropping:
Total WBC 0.2
HGB 6.9 (after blood)
Platelets 19K
So moving the right direction, and I need more blood today.
I got a triple infusion machine to be able to do chemo, antibiotics and blood all at the same time! :)
The plan now is to let the chemo do its thing. It will hang out in my body and for the next week work at destroying my current diseased bone marrow. In a week, they will check the bone marrow and if there's zero blasts in it, we'll consider that a success and I'll be able to let my normal blood cells repopulate my marrow and blood, and take a break till we give it another hit in a month. That, to me, is totally doable.
Unfortunately today as I thought about what *should* happen and what I *hope* will happen, I went to the other side, which is "it might not work this first time." The good news is that there is a way to determine if it was not effective and there is a treatment protocol to do something if it did not. And that's going to improve the ultimate goal of achieving minimal residual disease. Here's a great handout on MRD in blood cancers, although I'm not sure why it doesn't include AML specifically. I *think* using MRD for AML is still evolving, so maybe that's why it's only in PubMed and not on the general L&LS or ACS pages.
At any rate, I obviously would love a complete response this first time through, which might actually allow me to go home for Xmas. So if you would like something to do over the next week, I invite you join me in visualizing the chemo trashing the shit out of my bone marrow. You can do it however you want. Here's an image of blood entering bone marrow, and the chemo is in my blood, so that can work:
You can imagine the chemo clearing everything that shouldn't be there in the blood throughout the body, including the bone marrow, and flushing it out of my body/kidneys (maybe a teenaged boy visual...)
Or you can make up a cartoon or imagery that helps you imagine what's happening.
Lots of people use pac-man visuals for chemo, gobbling up cancerous cells
You can imagine a warrior or a boxer or any number of violent cultural references.
Or you can use what I used to get through breast cancer chemo: Buffy the Vampire Slayer staking. I especially like this one because it's not just Buffy, but all those who love her fighting off the bad stuff. Also, when she stakes, the vampires go up into dust, which is just an awesome visual, I think.
If you think of another one, or had your own chemo visual during treatment, let me know!
Here's to completion of the first phase. Thank you all for following along.
Counts still dropping:
Total WBC 0.2
HGB 6.9 (after blood)
Platelets 19K
So moving the right direction, and I need more blood today.
I got a triple infusion machine to be able to do chemo, antibiotics and blood all at the same time! :)
The plan now is to let the chemo do its thing. It will hang out in my body and for the next week work at destroying my current diseased bone marrow. In a week, they will check the bone marrow and if there's zero blasts in it, we'll consider that a success and I'll be able to let my normal blood cells repopulate my marrow and blood, and take a break till we give it another hit in a month. That, to me, is totally doable.
Unfortunately today as I thought about what *should* happen and what I *hope* will happen, I went to the other side, which is "it might not work this first time." The good news is that there is a way to determine if it was not effective and there is a treatment protocol to do something if it did not. And that's going to improve the ultimate goal of achieving minimal residual disease. Here's a great handout on MRD in blood cancers, although I'm not sure why it doesn't include AML specifically. I *think* using MRD for AML is still evolving, so maybe that's why it's only in PubMed and not on the general L&LS or ACS pages.
At any rate, I obviously would love a complete response this first time through, which might actually allow me to go home for Xmas. So if you would like something to do over the next week, I invite you join me in visualizing the chemo trashing the shit out of my bone marrow. You can do it however you want. Here's an image of blood entering bone marrow, and the chemo is in my blood, so that can work:
You can imagine the chemo clearing everything that shouldn't be there in the blood throughout the body, including the bone marrow, and flushing it out of my body/kidneys (maybe a teenaged boy visual...)
Or you can make up a cartoon or imagery that helps you imagine what's happening.
Lots of people use pac-man visuals for chemo, gobbling up cancerous cells
You can imagine a warrior or a boxer or any number of violent cultural references.
Or you can use what I used to get through breast cancer chemo: Buffy the Vampire Slayer staking. I especially like this one because it's not just Buffy, but all those who love her fighting off the bad stuff. Also, when she stakes, the vampires go up into dust, which is just an awesome visual, I think.
If you think of another one, or had your own chemo visual during treatment, let me know!
Here's to completion of the first phase. Thank you all for following along.
Thursday, December 5, 2019
Meds and tests and giving in to medicine
I thought I'd start by putting my numbers from my blood counts over the last few days here. Although I wrote about what the tests measure and indicate, I didn't give all the numbers I had.
Copying from my last post to get the general range of numbers, I'll put in my numbers after. I have labs run every morning (between 3:30 and 6:00 am).
Total white blood cell count
Normal is 4.2-11.0
5.0, 5.1, 6.9, 4.1, 6.3, 5.4, 2.5, 1.1, 0.4
Hemoglobin
Normal is 12-15.5
They will do a whole blood transfusion if it drops below 7.0
8.6, 8.2, 9.5, 8.0, 7.4, 7.6, 7.8, 6.5
Platelets
Normal is 140K-450K, but mine have never been that high
They will do a platelet transfusion if it drops below 10K
23K, 21K, 38K, 22K, 20K, 18K, 15K, 10K, 5K
Absolute neutrophils
Normal is 1.8-7.7
They call it neutropenic if I drop below 1.5, and exercise additional precautions, including putting me on a prophylactic antibiotic; apparently once you're declared neutropenic, they stop running this and the blast percentage because the total WBC count is so low that it's really hard to get fractions.
1.1, 0.8, 1.7, 1.8, 4.3, 4.2, 1.6, 0.4...
Blast percentage
Normal is 1-5% in bone marrow, but none in blood; this goes along with the neutropenic marker and is no longer run after you go neutropenic.
42%, 28%, 10%, 2%, 14%, 12%
What this means is that today I will get a blood transfusion and also platelets. I am indebted to all who are able to donate, as it truly will save my life. I'm also a little bit scared as the consent form lists things that could potentially happen if you receive blood from another person. Still, I don't exactly have another option, so we'll do it!
Last night was a rough night. As my blood cells dropped, I started to develop a fever. I also was ridiculously exhausted--to the point of not being able to keep my eyes open. It was kind of scary to be that out of it, but also strangely nice to not be able to do anything other than just sleep. My temp started to creep up into the 100's and I was warned that if it hit 101.5 they'd have to do all sorts of thing, including preventative antibiotics and a bunch of tests to make sure it wasn't an infection causing the fever. I have always been the kind of person who spiked fevers easily (My mom used to say, "you get a fever from a paper cut."). So part of me knew that this was likely my body reacting to all the crap being thrown at it. But it's still scary when they're doing all sorts of things, "just in case." And then my temp hit 101.8.
I spent over 12 hours drifting in and out of consciousness (sleepy-consciousness) while my vitals were taken over and over, I was given meds, and more blood was drawn and more other things sampled, and I got an X-ray in my hospital room...
At this point the urinalysis and the X-ray were both negative for anything, but it can take days for the blood cultures to come back. The longer w/o results, the better in that case, meaning nothing is growing. Again, I'm hoping it's just my body and the way it reacts to any trauma and not another thing to have to deal with.
---------------------------------
I asked my nurse this morning to go over all the meds I'm on, and explain them. Here we go:
Idarubicin: chemo given daily for 3 days; done with this one
Cytarabine: chemo given around the clock for 7+ days (there's some extension of time with the IV bags and changes of lines and such, so it ends up being over 7 days; I'm still getting this one and it is due to end sometime on Saturday.
Posaconazole: oral med that is an anti-fungal
Allopurinol: oral med to decrease uric acid, which can increase with the chemo as cancer cells die, and it ultimately protects my kidneys
Ondansetrone/Zofram: anti-nausea meds given in my IV
Cephapine--IV antibiotic given when neutrophils drop
Vancomycin--second IV antibiotic added when my temp went over 101.5
Femara/Letrozole: the aromatase inhibitor that I have been on for four years already
Calcium/Vit D.: vitamins I've taken for a long time
Acyclovir: Anti-viral that will be added when the chemo is done
I was taken back 25 years when I was writing my birth plan and was ADAMANT that I would not get an IV placed because it was too invasive. I didn't want pain meds for labor or pitocin for induction. I wanted to trust my body to de exactly what it was made to do.
It's insane to think about that now. Central lines, additional IVs as needed, a med list that I can't remember and have to write down. Everything going into me and coming out of me being measured... What I wouldn't give to just have to defend my birth plan now!
---------------------
I'm gearing up for another day of hard work. I need to try to walk or otherwise exercise since I barely did anything yesterday. I'll have 1-1.5 hours of platelet transfusion, then 2.5-3 hours of blood transfusion. I'm tired, but I'm not so completely exhausted as I was yesterday. I have been told that it will get worse before it gets better, and I'm still moving forward. Two more days of chemo, and I just keep checking things off the list.
While it's been nice to see people, it really wipes me out, so please don't be offended if you ask to visit and I just can't do it. It's taken an inordinately long time to be able to type this blog post since I'm super easily distracted. I had thought I'd be able to keep up with work while I was hospitalized. While I can do tiny bits, I can't sustain thoughts or plans. So I guess resting is where it's at. (And walking. So much walking.)
Copying from my last post to get the general range of numbers, I'll put in my numbers after. I have labs run every morning (between 3:30 and 6:00 am).
Total white blood cell count
Normal is 4.2-11.0
5.0, 5.1, 6.9, 4.1, 6.3, 5.4, 2.5, 1.1, 0.4
Hemoglobin
Normal is 12-15.5
They will do a whole blood transfusion if it drops below 7.0
8.6, 8.2, 9.5, 8.0, 7.4, 7.6, 7.8, 6.5
Platelets
Normal is 140K-450K, but mine have never been that high
They will do a platelet transfusion if it drops below 10K
23K, 21K, 38K, 22K, 20K, 18K, 15K, 10K, 5K
Absolute neutrophils
Normal is 1.8-7.7
They call it neutropenic if I drop below 1.5, and exercise additional precautions, including putting me on a prophylactic antibiotic; apparently once you're declared neutropenic, they stop running this and the blast percentage because the total WBC count is so low that it's really hard to get fractions.
1.1, 0.8, 1.7, 1.8, 4.3, 4.2, 1.6, 0.4...
Blast percentage
Normal is 1-5% in bone marrow, but none in blood; this goes along with the neutropenic marker and is no longer run after you go neutropenic.
42%, 28%, 10%, 2%, 14%, 12%
What this means is that today I will get a blood transfusion and also platelets. I am indebted to all who are able to donate, as it truly will save my life. I'm also a little bit scared as the consent form lists things that could potentially happen if you receive blood from another person. Still, I don't exactly have another option, so we'll do it!
----------------------------------------------
I spent over 12 hours drifting in and out of consciousness (sleepy-consciousness) while my vitals were taken over and over, I was given meds, and more blood was drawn and more other things sampled, and I got an X-ray in my hospital room...
At this point the urinalysis and the X-ray were both negative for anything, but it can take days for the blood cultures to come back. The longer w/o results, the better in that case, meaning nothing is growing. Again, I'm hoping it's just my body and the way it reacts to any trauma and not another thing to have to deal with.
---------------------------------
I asked my nurse this morning to go over all the meds I'm on, and explain them. Here we go:
Idarubicin: chemo given daily for 3 days; done with this one
Cytarabine: chemo given around the clock for 7+ days (there's some extension of time with the IV bags and changes of lines and such, so it ends up being over 7 days; I'm still getting this one and it is due to end sometime on Saturday.
Posaconazole: oral med that is an anti-fungal
Allopurinol: oral med to decrease uric acid, which can increase with the chemo as cancer cells die, and it ultimately protects my kidneys
Ondansetrone/Zofram: anti-nausea meds given in my IV
Cephapine--IV antibiotic given when neutrophils drop
Vancomycin--second IV antibiotic added when my temp went over 101.5
Femara/Letrozole: the aromatase inhibitor that I have been on for four years already
Calcium/Vit D.: vitamins I've taken for a long time
Acyclovir: Anti-viral that will be added when the chemo is done
I was taken back 25 years when I was writing my birth plan and was ADAMANT that I would not get an IV placed because it was too invasive. I didn't want pain meds for labor or pitocin for induction. I wanted to trust my body to de exactly what it was made to do.
It's insane to think about that now. Central lines, additional IVs as needed, a med list that I can't remember and have to write down. Everything going into me and coming out of me being measured... What I wouldn't give to just have to defend my birth plan now!
---------------------
I'm gearing up for another day of hard work. I need to try to walk or otherwise exercise since I barely did anything yesterday. I'll have 1-1.5 hours of platelet transfusion, then 2.5-3 hours of blood transfusion. I'm tired, but I'm not so completely exhausted as I was yesterday. I have been told that it will get worse before it gets better, and I'm still moving forward. Two more days of chemo, and I just keep checking things off the list.
While it's been nice to see people, it really wipes me out, so please don't be offended if you ask to visit and I just can't do it. It's taken an inordinately long time to be able to type this blog post since I'm super easily distracted. I had thought I'd be able to keep up with work while I was hospitalized. While I can do tiny bits, I can't sustain thoughts or plans. So I guess resting is where it's at. (And walking. So much walking.)
Wednesday, December 4, 2019
A slave to the numbers
I missed posting yesterday on the one week anniversary of my diagnosis (I'm kind of big with those kind of milestones--tomorrow will be the 5 year D-day/official diagnosis of my breast cancer). Man, the holiday season seems to suck for this kind of stuff.
Anyway, I've been settling into a sort of pattern. Everyone here is wonderful, but the fact of the matter is that there is a lot of interruption that must occur in the hospital, and especially on the oncology wing. The good news is that, as I've gotten more sleep-deprived, the hospital bed is less uncomfortable and I'm actually sleeping some. The weaning of the steroids has undoubtedly helped as well (I only got those before the three doses of Idarubicin).
I have always tracked my lab counts ad nauseam and one of the nurses here told me a few days ago which numbers I really need to track, and also said that she can get the results before they appear on my medical record that I can access myself. So they keep giving me my counts. I hope I'm understanding and correctly sharing the meaning of each, but I may have to edit.
Here's what they're following:
Total white blood cell count
Normal is 4.2-11.0
If below 1, it's a greatly-increased risk of infection
We want to see this go down, as it shows that the chemo is majorly messing up the bone marrow and keeping it from making white blood cells (infection fighters) which are what caused this overgrowth in the first place
Hemoglobin
Normal is 12-15.5
They will do a whole blood transfusion if it drops below 7.0
Hemoglobin is a protein that is responsible for making red blood cells carry oxygen to the cells (as all cells need oxygen). Low hemoglobin results in anemia. This will undoubtedly go down, so there will be transfusions in my future. I've never had one, but apparently they do make you feel better when you get one.
Platelets
Normal is 140K-450K, but mine have never been that high
They will do a platelet transfusion if it drops below 10K
Platelets are responsible for clotting of the blood, and so it's important to have enough to clot if anything internal or external causes a bleed. As I get more exhausted, falling is more likely (ie: could bleed internally) and I have so many things connected to my skin that external bleeds are also more likely. I did need one platelet transfusion after my mastectomy, and I guess I handled it fine.
Absolute neutrophils
Normal is 1.8-7.7
They call it neutropenic if I drop below 1.5, and exercise additional precautions, including putting me on a prophylactic antibiotic.
Neutrophils are the first line of defense in an infection, so something that would normally be fought off by a healthy person (ie: ear infection) can almost immediately become septic. It may be an overabundance of caution, but I've chosen, with my team's support, to require everyone to mask up now that my levels are low even if they don't have symptoms. It's just not worth the risk.
Blast percentage
Normal is 1-5% in bone marrow, but none in blood
Blasts are partially-differentiated hematopoietic stem cells that populate the white blood cell (infection-fighting) line. In leukemia, they divide uncontrolled (cancer thing) and fill up the bone marrow, preventing effective blood cells of all types to be formed. In leukemia they also spill out into the blood and can be viewed and measured that way. That's how my initial diagnosis at Dr. Shah's office was made. There should be under 5% blasts at any time, and more than 20% are sufficient to diagnose that some sort of leukemia is happening. Mine were 30% in Dr. Shah's office.
So I've been tracking my numbers and while my blasts were trending downward, yesterday they took an uptick, which completely freaked me out. Being mostly stuck in a hospital bed with only your own thoughts (and the internet) is not a great way to be reasonable. Suffice to say that my blasts had gotten down to 2% and then yesterday shot up to 14% (thus the panic) but are heading back down, being 12% today. And that's what we want because it means that the chemo is working. If you want to visualize or vibe or pray, feel free to work on dropping those blasts!
But Dr. Thompson was happy that the other blood counts are all about where they should be. He said an increase in WBC would not be good now, and they are definitely trending down. Neither my hemoglobin nor platelets were low enough for transfusions today--although it's always possible tomorrow. Slow and steady.
I had been able to sleep significantly more last night, and had a hard time waking up this morning. Then late this morning I could barely keep my eyes open. It's got to be the cell counts, and the absence of steroids. I had some people who were going to visit and I had to turn them away. My eyes were rolling back in my head I was so sleepy.
And as I was napping, I felt like I was running a fever. I have always had chills and body aches with low grade fevers since I was a kid. I wasn't sure whether to say or do anything because I was already getting antibiotic in my IV since my neutrophils had fallen so low. At routine vitals, it was found that I had a temperature over 100. It was explained that they'd watch, but if my temp got to 101.5, then the big guns/protections would be pulled in. I'd need blood cultures--from the port but also peripheral. I'd need a urinalysis. And then a chest X-ray--all to insure that the fever was from the chemo but not an infection. I was shivering and the nurses turned up the heat in the room and I put on some fuzzy socks and more blankets. I stopped shivering, but my temp eased up to 101.3. And an hour later, it was at 101.4. The nurse put in a call to the doctor to get things going. :( And then I pried myself out of bed and Greg walked me around the floor. It was tough to keep moving and I just wanted nothing more than to crawl into bed and sleep, but it worked. My temp went back down to 100.8 and just now it was 100.0. I have to remember there's a such thing as too warm!
Not much else to report. I feel like my brain is quite foggy and it's hard to hold a conversation, so if you do come visit, know that I may not make sense. I'm glad I started this blog post awhile before I crashed. I still don't know if I was correct in all that I wrote, but I hope it made a little sense.
Oh, the other big thing that happened today is that I was able to trash the Tele (EKG telemetry). Everyone has to be monitored for a little while, and I'd been doing pretty well but then I think I actually moved in a strange way and caused an irregular heartbeat (v-tach) and so I was kept on the Tele. I did create a game with it where I walk around the floor and whenever there is a display, I seek out my name and measurement and try to get it to settle down and have a normal pattern. After that, I started playing the 87 game--I'd breathe slowly and steadily to try to bring my heart rate down to 87 (because Class of 87 rules...). It broke up my walks.
but it also meant that I had six electrodes stuck to my chest and a heavy transponder to carry around with me. I was pretty happy to say goodbye to the Tele.
And I am almost 5 days into the 7 day chemo regimen. I know it'll be a little longer and it's possible it'll be a LOT longer, but I'm moving forward. Here's hoping those numbers stay/move where they are supposed to be, and I rebound at least a little bit in energy. For now, I think I'm going to take a 7:00 pm nap...
Anyway, I've been settling into a sort of pattern. Everyone here is wonderful, but the fact of the matter is that there is a lot of interruption that must occur in the hospital, and especially on the oncology wing. The good news is that, as I've gotten more sleep-deprived, the hospital bed is less uncomfortable and I'm actually sleeping some. The weaning of the steroids has undoubtedly helped as well (I only got those before the three doses of Idarubicin).
I have always tracked my lab counts ad nauseam and one of the nurses here told me a few days ago which numbers I really need to track, and also said that she can get the results before they appear on my medical record that I can access myself. So they keep giving me my counts. I hope I'm understanding and correctly sharing the meaning of each, but I may have to edit.
Here's what they're following:
Total white blood cell count
Normal is 4.2-11.0
If below 1, it's a greatly-increased risk of infection
We want to see this go down, as it shows that the chemo is majorly messing up the bone marrow and keeping it from making white blood cells (infection fighters) which are what caused this overgrowth in the first place
Hemoglobin
Normal is 12-15.5
They will do a whole blood transfusion if it drops below 7.0
Hemoglobin is a protein that is responsible for making red blood cells carry oxygen to the cells (as all cells need oxygen). Low hemoglobin results in anemia. This will undoubtedly go down, so there will be transfusions in my future. I've never had one, but apparently they do make you feel better when you get one.
Platelets
Normal is 140K-450K, but mine have never been that high
They will do a platelet transfusion if it drops below 10K
Platelets are responsible for clotting of the blood, and so it's important to have enough to clot if anything internal or external causes a bleed. As I get more exhausted, falling is more likely (ie: could bleed internally) and I have so many things connected to my skin that external bleeds are also more likely. I did need one platelet transfusion after my mastectomy, and I guess I handled it fine.
Absolute neutrophils
Normal is 1.8-7.7
They call it neutropenic if I drop below 1.5, and exercise additional precautions, including putting me on a prophylactic antibiotic.
Neutrophils are the first line of defense in an infection, so something that would normally be fought off by a healthy person (ie: ear infection) can almost immediately become septic. It may be an overabundance of caution, but I've chosen, with my team's support, to require everyone to mask up now that my levels are low even if they don't have symptoms. It's just not worth the risk.
Blast percentage
Normal is 1-5% in bone marrow, but none in blood
Blasts are partially-differentiated hematopoietic stem cells that populate the white blood cell (infection-fighting) line. In leukemia, they divide uncontrolled (cancer thing) and fill up the bone marrow, preventing effective blood cells of all types to be formed. In leukemia they also spill out into the blood and can be viewed and measured that way. That's how my initial diagnosis at Dr. Shah's office was made. There should be under 5% blasts at any time, and more than 20% are sufficient to diagnose that some sort of leukemia is happening. Mine were 30% in Dr. Shah's office.
So I've been tracking my numbers and while my blasts were trending downward, yesterday they took an uptick, which completely freaked me out. Being mostly stuck in a hospital bed with only your own thoughts (and the internet) is not a great way to be reasonable. Suffice to say that my blasts had gotten down to 2% and then yesterday shot up to 14% (thus the panic) but are heading back down, being 12% today. And that's what we want because it means that the chemo is working. If you want to visualize or vibe or pray, feel free to work on dropping those blasts!
But Dr. Thompson was happy that the other blood counts are all about where they should be. He said an increase in WBC would not be good now, and they are definitely trending down. Neither my hemoglobin nor platelets were low enough for transfusions today--although it's always possible tomorrow. Slow and steady.
I had been able to sleep significantly more last night, and had a hard time waking up this morning. Then late this morning I could barely keep my eyes open. It's got to be the cell counts, and the absence of steroids. I had some people who were going to visit and I had to turn them away. My eyes were rolling back in my head I was so sleepy.
And as I was napping, I felt like I was running a fever. I have always had chills and body aches with low grade fevers since I was a kid. I wasn't sure whether to say or do anything because I was already getting antibiotic in my IV since my neutrophils had fallen so low. At routine vitals, it was found that I had a temperature over 100. It was explained that they'd watch, but if my temp got to 101.5, then the big guns/protections would be pulled in. I'd need blood cultures--from the port but also peripheral. I'd need a urinalysis. And then a chest X-ray--all to insure that the fever was from the chemo but not an infection. I was shivering and the nurses turned up the heat in the room and I put on some fuzzy socks and more blankets. I stopped shivering, but my temp eased up to 101.3. And an hour later, it was at 101.4. The nurse put in a call to the doctor to get things going. :( And then I pried myself out of bed and Greg walked me around the floor. It was tough to keep moving and I just wanted nothing more than to crawl into bed and sleep, but it worked. My temp went back down to 100.8 and just now it was 100.0. I have to remember there's a such thing as too warm!
Not much else to report. I feel like my brain is quite foggy and it's hard to hold a conversation, so if you do come visit, know that I may not make sense. I'm glad I started this blog post awhile before I crashed. I still don't know if I was correct in all that I wrote, but I hope it made a little sense.
Oh, the other big thing that happened today is that I was able to trash the Tele (EKG telemetry). Everyone has to be monitored for a little while, and I'd been doing pretty well but then I think I actually moved in a strange way and caused an irregular heartbeat (v-tach) and so I was kept on the Tele. I did create a game with it where I walk around the floor and whenever there is a display, I seek out my name and measurement and try to get it to settle down and have a normal pattern. After that, I started playing the 87 game--I'd breathe slowly and steadily to try to bring my heart rate down to 87 (because Class of 87 rules...). It broke up my walks.
but it also meant that I had six electrodes stuck to my chest and a heavy transponder to carry around with me. I was pretty happy to say goodbye to the Tele.
And I am almost 5 days into the 7 day chemo regimen. I know it'll be a little longer and it's possible it'll be a LOT longer, but I'm moving forward. Here's hoping those numbers stay/move where they are supposed to be, and I rebound at least a little bit in energy. For now, I think I'm going to take a 7:00 pm nap...
Sunday, December 1, 2019
The bullet train
When I was still figuring out my breast cancer diagnosis five years ago, my survivor friend Dawn told me to jump on the breast cancer train, as one thing (a lump) leads to another (a mammogram) and another (an ultrasound) and another (a biopsy), etc. and that if it was really cancer, it would build to a bullet train. I love Dawn and her analogy, but in retrospect, that was not a bullet train. There was plenty of time to stop, think, worry, have sleepless nights, etc. But the leukemia train? That is a freaking bullet train.
Tuesday at my 6 month checkup, Dr. Shah handed me a slip of paper with a referral, because her hospital system does not have any leukemia oncologists. She told me they would be expecting my call and to make sure my phone was charged and on "ring" and that I needed to go see the referral doctor TOMORROW MORNING and be ready to be admitted. The only problem is that this doctor belongs to a hospital system that our insurance does not cover. When I told Dr. Shah this, she said that there is no other specialist in the area and that I should talk to my insurance company to figure out how to make it work. So while waiting for Greg to arrive, I'm on one phone with the specialist who is not covered, trying to find out if I can get an out-of-network exception pushed through by their hospital, and another phone trying to explain to my insurance company that I have to be seen OON because there is no other specialist in the area. Neither of these calls went well.
Fast forward to a few hours later when my Team Phoenix sister Barb came to the rescue, called everyone she could within the Aurora network and got me the names for the most highly recommended doctors in the Aurora system (in network) who DO treat leukemia patients. I shared their names with Dr. Shah, she called and transferred records, and told me that I needed to go right away to St. Luke's emergency department which would be the "easiest" way to get me into the hospital where I needed to be. And she told me to pack as if I'd be staying a long time.
The St. Luke's emergency department was, of course, full of germy kids, people coughing, moaning, etc. And I had just found out that I was pretty severely immunocompromised. I grabbed a mask.
After 8 hours in the emergency department, a whole lot of blood draws--some successful, others not so much, and exposure to some interesting patients, I had a room on the oncology floor. I sent Greg home around 11:00 pm and got all my admission stuff done. And then I tried (unsuccessfully) to sleep.
Wednesday was a whirlwind of provider visits and pre-admission tests. The hospitalist, the hematological oncologist on duty, the cardiac oncology department, the infectious disease specialist, associated Nurse Practitioners, and nurses and nursing assistants and phlebotomists and on and on. And Meredith came to visit:
She sat with Greg while I had my bone marrow biopsy, my echocardiogram, and my chest x-ray. And then, because my blood counts weren't frighteningly low and because I was put on a protective antibiotic, I was able to go home and sleep in my own bed for two days, have thanksgiving with my extended family, and love on all three of my kids, including putting up the Christmas tree.
Friday we went to the outpatient clinic for labs and an appointment at noon. I got my definitive diagnosis of treatment-related acute myeloid leukemia (t-AML). They do genetic testing on the bone marrow that takes longer and it can tell what kind of mutations caused the leukemia. However, the fact that this is treatment-related already escalates it to a more severe case. I was told to walk across the skywalk and be admitted to in-patient at St. Luke's. I was packed and better prepared this time.
I got a slightly different room with a slightly less desirable view, but my luck continues with excellent staff all around. I've been hospitalized before and I spent a lot of time with my mom during her hospitalizations and there is often some staff member (usually a night nurse) who is not the most agreeable person. I have not found one difficult staff member yet here at St. Luke's. They are amazing and positive and friendly and willing to answer my millions of questions at the level I can comprehend. And they repeat things when I forget or need clarification. I feel very confident that I'm where I should be.
So now the treatment plan, which is, of course subject to change along the way. It seems to follow pretty closely the treatment guidelines that the ACS spells out.
3. Consolidation: I will come back to the hospital four more times, once every four weeks, to get more high-dose infusions with Cytarabine. This will hopefully knock out any remaining leukemic cells that made it through the initial intense phase.
For some low risk cases of AML, this is all the treatment that is needed, and a person's immune system essentially gets jump-started back to normal. But given that this is t-AML (and we don't yet know the genetic markers), it's treated as higher risk, and the next step is:
4. Bone marrow transplant: I'm not a candidate for autologous stem cell transplant (from yourself), so this will be an allogenic (donor) transplant. Siblings are the best chance for a match, but they're only about a 50% chance. I have high hopes that my brother is more like me than he thinks. :) If he's not a match, I'm not sure if they look to other relatives first or just open it to an anonymous donor. That won't happen until spring/summer, so I haven't focused too much on it.
----------------------------
Whew! That's a lot. I cannot believe I've only known about this less than five days and am already this deep in. Truly a bullet train. In many ways it's been easier than with my breast cancer diagnosis because there's been no time to think--just to act. But it's also scarier--both because I've done something like this before, so I know how crappy it's going to be; but also because this is a bigger deal. And I only know one person who has done this, so I don't have as many people to draw on their experiences. I don't like uncertainty!
I do have some positives going for me. I'm “young” (defined as under 60). I’m in pretty good physical shape (thank you, Team Phoenix, Cadence, and my Fat Biking buddies!). My heart function tests apparently came back really good, despite being on two cardiotoxic drugs with my BC treatment. All my other tests (kidney and liver function, electrolytes, x-ray, communicable disease, etc.) are great. My blood pressure, EKG, pulse ox, etc. all look great. My appetite has returned (hello, steroid pre-meds) and they encourage walking the hall (have to stay on the oncology floor) and have exercise bikes out for patient use. I'll be doing my best to stay as fit as can be so I can be back on a real bike as soon as I have enough platelets to do so!
-----------------------------
As people have found out about this, they've all been so supportive with positive thoughts and offers to help. At this point, I don't think we need anything in terms of help with meals or anything like that. I'll be in the hospital, being taken care of, and only Greg and Ash are home. They'll have two cars so able to get themselves around. And they're both in and out, busy with so many things. I'm sure there will be a lot of frozen pizza or other quick/take-out meals, and that's fine. Cara will be back from grad school in two weeks and she's excited to cook in a real kitchen and generally take care of us all. Travis will probably be home a week after that. And Ash has always been immensely independent and able to cook and clean and help with everything. I made some awesome kids and chose a fantastic life partner.
I will try to keep up with this blog to send out bigger updates (or just to entertain myself with all my hospital time). I'll put little updates on Facebook. My dear Team Phoenix sister Meredith has offered to organize visits if it comes to that. At this point I am free to have company, and after today I'll have less family company, so happy to have visitors, especially during week days--as long as you're not sick and haven't been around someone sick. I'd ask that you text me before coming in case I'm particularly exhausted or if like five people want to come at once. And I may reserve the right to send you to Meredith to organize. :) I cannot have any plants or flowers (germs). I have to be careful with foods brought in. So no gifts--just company and emails or texts or messages. As with the breast cancer journey, I know it's my friends and their positive energy that got me through as well as I did. I'm hoping for the same this time.
And if you really want to DO something, please donate blood or platelets. I'll be drawing a LOT from the stores that currently exist. I'd feel better if they weren't depleted. And if you do, let me know. I'll thank you profusely.
May I also suggest that sign up for "Be the match"? If you are between the ages of 18 and 44, your bone marrow is more effective in a transplant. You don't have to donate anything (other than a cheek swab, I think) unless you're matched with someone. You could literally save a life.
OK, let's do this thing!
Tuesday at my 6 month checkup, Dr. Shah handed me a slip of paper with a referral, because her hospital system does not have any leukemia oncologists. She told me they would be expecting my call and to make sure my phone was charged and on "ring" and that I needed to go see the referral doctor TOMORROW MORNING and be ready to be admitted. The only problem is that this doctor belongs to a hospital system that our insurance does not cover. When I told Dr. Shah this, she said that there is no other specialist in the area and that I should talk to my insurance company to figure out how to make it work. So while waiting for Greg to arrive, I'm on one phone with the specialist who is not covered, trying to find out if I can get an out-of-network exception pushed through by their hospital, and another phone trying to explain to my insurance company that I have to be seen OON because there is no other specialist in the area. Neither of these calls went well.
Fast forward to a few hours later when my Team Phoenix sister Barb came to the rescue, called everyone she could within the Aurora network and got me the names for the most highly recommended doctors in the Aurora system (in network) who DO treat leukemia patients. I shared their names with Dr. Shah, she called and transferred records, and told me that I needed to go right away to St. Luke's emergency department which would be the "easiest" way to get me into the hospital where I needed to be. And she told me to pack as if I'd be staying a long time.
The St. Luke's emergency department was, of course, full of germy kids, people coughing, moaning, etc. And I had just found out that I was pretty severely immunocompromised. I grabbed a mask.
After 8 hours in the emergency department, a whole lot of blood draws--some successful, others not so much, and exposure to some interesting patients, I had a room on the oncology floor. I sent Greg home around 11:00 pm and got all my admission stuff done. And then I tried (unsuccessfully) to sleep.
Wednesday was a whirlwind of provider visits and pre-admission tests. The hospitalist, the hematological oncologist on duty, the cardiac oncology department, the infectious disease specialist, associated Nurse Practitioners, and nurses and nursing assistants and phlebotomists and on and on. And Meredith came to visit:
She sat with Greg while I had my bone marrow biopsy, my echocardiogram, and my chest x-ray. And then, because my blood counts weren't frighteningly low and because I was put on a protective antibiotic, I was able to go home and sleep in my own bed for two days, have thanksgiving with my extended family, and love on all three of my kids, including putting up the Christmas tree.
Friday we went to the outpatient clinic for labs and an appointment at noon. I got my definitive diagnosis of treatment-related acute myeloid leukemia (t-AML). They do genetic testing on the bone marrow that takes longer and it can tell what kind of mutations caused the leukemia. However, the fact that this is treatment-related already escalates it to a more severe case. I was told to walk across the skywalk and be admitted to in-patient at St. Luke's. I was packed and better prepared this time.
I got a slightly different room with a slightly less desirable view, but my luck continues with excellent staff all around. I've been hospitalized before and I spent a lot of time with my mom during her hospitalizations and there is often some staff member (usually a night nurse) who is not the most agreeable person. I have not found one difficult staff member yet here at St. Luke's. They are amazing and positive and friendly and willing to answer my millions of questions at the level I can comprehend. And they repeat things when I forget or need clarification. I feel very confident that I'm where I should be.
So now the treatment plan, which is, of course subject to change along the way. It seems to follow pretty closely the treatment guidelines that the ACS spells out.
- Chemo to induce remission: I got in the hospital Friday afternoon, had my picc line inserted, and started chemo that night. It wasn't until I was reading later that I understood the urgency. Apparently survival of untreated AML is "measured in days or weeks."

so much better than being poked over and over - Regimen includes:
- Three Idarubacin infusions of 15 minutes apiece over three days. This is an anthracycline similar to Adriamycin (the red devil) which I received for breast cancer treatment. It's reddish orange and kind of scary looking. I have completed two of the three.
2. Continuous (24 hours) infusion of Cytarabine for seven days straight.
My best friend, the IV pole
3. Consolidation: I will come back to the hospital four more times, once every four weeks, to get more high-dose infusions with Cytarabine. This will hopefully knock out any remaining leukemic cells that made it through the initial intense phase.
For some low risk cases of AML, this is all the treatment that is needed, and a person's immune system essentially gets jump-started back to normal. But given that this is t-AML (and we don't yet know the genetic markers), it's treated as higher risk, and the next step is:
4. Bone marrow transplant: I'm not a candidate for autologous stem cell transplant (from yourself), so this will be an allogenic (donor) transplant. Siblings are the best chance for a match, but they're only about a 50% chance. I have high hopes that my brother is more like me than he thinks. :) If he's not a match, I'm not sure if they look to other relatives first or just open it to an anonymous donor. That won't happen until spring/summer, so I haven't focused too much on it.
----------------------------
Whew! That's a lot. I cannot believe I've only known about this less than five days and am already this deep in. Truly a bullet train. In many ways it's been easier than with my breast cancer diagnosis because there's been no time to think--just to act. But it's also scarier--both because I've done something like this before, so I know how crappy it's going to be; but also because this is a bigger deal. And I only know one person who has done this, so I don't have as many people to draw on their experiences. I don't like uncertainty!
I do have some positives going for me. I'm “young” (defined as under 60). I’m in pretty good physical shape (thank you, Team Phoenix, Cadence, and my Fat Biking buddies!). My heart function tests apparently came back really good, despite being on two cardiotoxic drugs with my BC treatment. All my other tests (kidney and liver function, electrolytes, x-ray, communicable disease, etc.) are great. My blood pressure, EKG, pulse ox, etc. all look great. My appetite has returned (hello, steroid pre-meds) and they encourage walking the hall (have to stay on the oncology floor) and have exercise bikes out for patient use. I'll be doing my best to stay as fit as can be so I can be back on a real bike as soon as I have enough platelets to do so!
-----------------------------
As people have found out about this, they've all been so supportive with positive thoughts and offers to help. At this point, I don't think we need anything in terms of help with meals or anything like that. I'll be in the hospital, being taken care of, and only Greg and Ash are home. They'll have two cars so able to get themselves around. And they're both in and out, busy with so many things. I'm sure there will be a lot of frozen pizza or other quick/take-out meals, and that's fine. Cara will be back from grad school in two weeks and she's excited to cook in a real kitchen and generally take care of us all. Travis will probably be home a week after that. And Ash has always been immensely independent and able to cook and clean and help with everything. I made some awesome kids and chose a fantastic life partner.
I will try to keep up with this blog to send out bigger updates (or just to entertain myself with all my hospital time). I'll put little updates on Facebook. My dear Team Phoenix sister Meredith has offered to organize visits if it comes to that. At this point I am free to have company, and after today I'll have less family company, so happy to have visitors, especially during week days--as long as you're not sick and haven't been around someone sick. I'd ask that you text me before coming in case I'm particularly exhausted or if like five people want to come at once. And I may reserve the right to send you to Meredith to organize. :) I cannot have any plants or flowers (germs). I have to be careful with foods brought in. So no gifts--just company and emails or texts or messages. As with the breast cancer journey, I know it's my friends and their positive energy that got me through as well as I did. I'm hoping for the same this time.
And if you really want to DO something, please donate blood or platelets. I'll be drawing a LOT from the stores that currently exist. I'd feel better if they weren't depleted. And if you do, let me know. I'll thank you profusely.
May I also suggest that sign up for "Be the match"? If you are between the ages of 18 and 44, your bone marrow is more effective in a transplant. You don't have to donate anything (other than a cheek swab, I think) unless you're matched with someone. You could literally save a life.
OK, let's do this thing!
Subscribe to:
Posts (Atom)