When I was still figuring out my breast cancer diagnosis five years ago, my survivor friend Dawn told me to jump on the breast cancer train, as one thing (a lump) leads to another (a mammogram) and another (an ultrasound) and another (a biopsy), etc. and that if it was really cancer, it would build to a bullet train. I love Dawn and her analogy, but in retrospect, that was not a bullet train. There was plenty of time to stop, think, worry, have sleepless nights, etc. But the leukemia train? That is a freaking bullet train.
Tuesday at my 6 month checkup, Dr. Shah handed me a slip of paper with a referral, because her hospital system does not have any leukemia oncologists. She told me they would be expecting my call and to make sure my phone was charged and on "ring" and that I needed to go see the referral doctor TOMORROW MORNING and be ready to be admitted. The only problem is that this doctor belongs to a hospital system that our insurance does not cover. When I told Dr. Shah this, she said that there is no other specialist in the area and that I should talk to my insurance company to figure out how to make it work. So while waiting for Greg to arrive, I'm on one phone with the specialist who is not covered, trying to find out if I can get an out-of-network exception pushed through by their hospital, and another phone trying to explain to my insurance company that I have to be seen OON because there is no other specialist in the area. Neither of these calls went well.
Fast forward to a few hours later when my Team Phoenix sister Barb came to the rescue, called everyone she could within the Aurora network and got me the names for the most highly recommended doctors in the Aurora system (in network) who DO treat leukemia patients. I shared their names with Dr. Shah, she called and transferred records, and told me that I needed to go right away to St. Luke's emergency department which would be the "easiest" way to get me into the hospital where I needed to be. And she told me to pack as if I'd be staying a long time.
The St. Luke's emergency department was, of course, full of germy kids, people coughing, moaning, etc. And I had just found out that I was pretty severely immunocompromised. I grabbed a mask.
After 8 hours in the emergency department, a whole lot of blood draws--some successful, others not so much, and exposure to some interesting patients, I had a room on the oncology floor. I sent Greg home around 11:00 pm and got all my admission stuff done. And then I tried (unsuccessfully) to sleep.
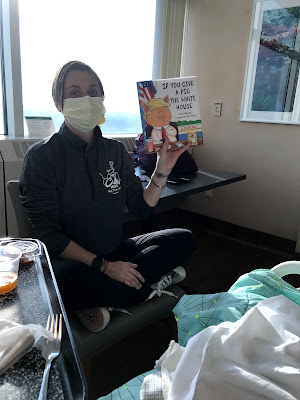
Wednesday was a whirlwind of provider visits and pre-admission tests. The hospitalist, the hematological oncologist on duty, the cardiac oncology department, the infectious disease specialist, associated Nurse Practitioners, and nurses and nursing assistants and phlebotomists and on and on. And Meredith came to visit:
She sat with Greg while I had my bone marrow biopsy, my echocardiogram, and my chest x-ray. And then, because my blood counts weren't frighteningly low and because I was put on a protective antibiotic, I was able to go home and sleep in my own bed for two days, have thanksgiving with my extended family, and love on all three of my kids, including putting up the Christmas tree.
Friday we went to the outpatient clinic for labs and an appointment at noon. I got my definitive diagnosis of treatment-related acute myeloid leukemia (t-AML). They do genetic testing on the bone marrow that takes longer and it can tell what kind of mutations caused the leukemia. However, the fact that this is treatment-related already escalates it to a more severe case. I was told to walk across the skywalk and be admitted to in-patient at St. Luke's. I was packed and better prepared this time.
I got a slightly different room with a slightly less desirable view, but my luck continues with excellent staff all around. I've been hospitalized before and I spent a lot of time with my mom during her hospitalizations and there is often some staff member (usually a night nurse) who is not the most agreeable person. I have not found one difficult staff member yet here at St. Luke's. They are amazing and positive and friendly and willing to answer my millions of questions at the level I can comprehend. And they repeat things when I forget or need clarification. I feel very confident that I'm where I should be.
So now the treatment plan, which is, of course subject to change along the way. It seems to follow pretty closely the treatment guidelines that the
ACS spells out.
- Chemo to induce remission: I got in the hospital Friday afternoon, had my picc line inserted, and started chemo that night. It wasn't until I was reading later that I understood the urgency. Apparently survival of untreated AML is "measured in days or weeks."
 |
| so much better than being poked over and over |
- Regimen includes:
- Three Idarubacin infusions of 15 minutes apiece over three days. This is an anthracycline similar to Adriamycin (the red devil) which I received for breast cancer treatment. It's reddish orange and kind of scary looking. I have completed two of the three.
 |
| My best friend, the IV pole |
2. Continuous (24 hours) infusion of Cytarabine for seven days straight.
These will hopefully knock out my defective bone marrow completely over those seven days. I will then stay in the hospital another 1-3 weeks while getting blood (if Hb < 7) and platelet (if <10K) transfusions and be monitored for infection and all the other fun medical stuff that can happen when you have no immune system. After one week, I'll have another bone marrow biopsy to see if the chemo actually knocked everything out (we hope that it did--I'll be asking for all your positive thoughts at that point). If it did NOT, I'll need more chemo to attempt to knock it all out. Either way, I will follow the intense period with
3.
Consolidation: I will come back to the hospital four more times, once every four weeks, to get more high-dose infusions with Cytarabine. This will hopefully knock out any remaining leukemic cells that made it through the initial intense phase.
For some low risk cases of AML, this is all the treatment that is needed, and a person's immune system essentially gets jump-started back to normal. But given that this is t-AML (and we don't yet know the genetic markers), it's treated as higher risk, and the next step is:
4.
Bone marrow transplant: I'm not a candidate for autologous stem cell transplant (from yourself), so this will be an allogenic (donor) transplant. Siblings are the best chance for a match, but they're only about a 50% chance. I have high hopes that my brother is more like me than he thinks. :) If he's not a match, I'm not sure if they look to other relatives first or just open it to an anonymous donor. That won't happen until spring/summer, so I haven't focused too much on it.
----------------------------
Whew! That's a lot. I cannot believe I've only known about this less than five days and am already this deep in. Truly a bullet train. In many ways it's been easier than with my breast cancer diagnosis because there's been no time to think--just to act. But it's also scarier--both because I've done something like this before, so I know how crappy it's going to be; but also because this is a bigger deal. And I only know one person who has done this, so I don't have as many people to draw on their experiences. I don't like uncertainty!
I do have some positives going for me. I'm “young” (defined as under 60). I’m in pretty good physical shape (thank you, Team Phoenix, Cadence, and my Fat Biking buddies!). My heart function tests apparently came back really good, despite being on two cardiotoxic drugs with my BC treatment. All my other tests (kidney and liver function, electrolytes, x-ray, communicable disease, etc.) are great. My blood pressure, EKG, pulse ox, etc. all look great. My appetite has returned (hello, steroid pre-meds) and they encourage walking the hall (have to stay on the oncology floor) and have exercise bikes out for patient use. I'll be doing my best to stay as fit as can be so I can be back on a real bike as soon as I have enough platelets to do so!
-----------------------------
As people have found out about this, they've all been so supportive with positive thoughts and offers to help. At this point, I don't think we need anything in terms of help with meals or anything like that. I'll be in the hospital, being taken care of, and only Greg and Ash are home. They'll have two cars so able to get themselves around. And they're both in and out, busy with so many things. I'm sure there will be a lot of frozen pizza or other quick/take-out meals, and that's fine. Cara will be back from grad school in two weeks and she's excited to cook in a real kitchen and generally take care of us all. Travis will probably be home a week after that. And Ash has always been immensely independent and able to cook and clean and help with everything. I made some awesome kids and chose a fantastic life partner.
I will try to keep up with this blog to send out bigger updates (or just to entertain myself with all my hospital time). I'll put little updates on Facebook. My dear Team Phoenix sister Meredith has offered to organize visits if it comes to that. At this point I am free to have company, and after today I'll have less family company, so happy to have visitors, especially during week days--as long as you're not sick and haven't been around someone sick. I'd ask that you text me before coming in case I'm particularly exhausted or if like five people want to come at once. And I may reserve the right to send you to Meredith to organize. :) I cannot have any plants or flowers (germs). I have to be careful with foods brought in. So no gifts--just company and emails or texts or messages. As with the breast cancer journey, I know it's my friends and their positive energy that got me through as well as I did. I'm hoping for the same this time.
And if you really want to DO something, please donate blood or platelets. I'll be drawing a LOT from the stores that currently exist. I'd feel better if they weren't depleted. And if you do, let me know. I'll thank you profusely.
May I also suggest that sign up for "
Be the match"? If you are between the ages of 18 and 44, your bone marrow is more effective in a transplant. You don't have to donate anything (other than a cheek swab, I think) unless you're matched with someone. You could literally save a life.
OK, let's do this thing!